Healthcare RCM Companies in USA
Healthcare RCM Companies in USA offer specialized revenue cycle management services that clinics, physician groups, and healthcare CFOs rely on to improve cash flow and reduce administrative burden. Choosing the right provider affects collections, coding accuracy, compliance, and patient satisfaction. This guide explains why clinics outsource RCM, how vendors work, technology differences, and what metrics to track.
Why clinics hire Healthcare RCM Companies in USA
Outsourcing revenue cycle tasks lets providers focus on care. Third-party teams handle claims, coding, payments, and denials while applying compliance controls and analytics. Clinics cite faster cash flow, fewer denials, improved ICD coding, and reduced administrative staffing costs as primary reasons to work with Healthcare RCM Companies in USA.
Common goals when outsourcing RCM
• Shorten days in A/R.
• Improve net collections.
• Reduce claim denials and rework.
• Ensure HIPAA-compliant processes.
• Adopt AI for coding and denial prevention.
What is RCM and how Healthcare RCM Companies in USA deliver it
Revenue cycle management (RCM) spans patient access through final payment posting. Healthcare RCM Companies in USA typically manage:
Intake & patient access
Verify insurance, pre-authorizations, and collect copays. Accurate insurance verification lowers rejected claims and improves patient financial clarity. Services such as Insurance Payment Verification Services are critical here.
Coding & claims preparation
Professional coders and automated ICD tools convert clinical documentation into claim-ready codes. Many vendors combine human review with tools such as an Automated ICD Coding Tool with AI for speed and accuracy. Mention of IPDRG and ICD standards helps reduce miscoding risks.
Claims submission & follow-up
Claims move through payer portals or clearinghouses. Healthcare RCM Companies in USA use rule-driven scrubbing to reduce denials before submission and active follow-up workflows afterward.
Payment posting & reconciliation
Accurate posting ensures clean financial records and quick denial triggers. Timely payment posting lets practices spot underpayments and begin appeals faster.
Denial management & appeals
Denial Prediction and Prevention Services identify high-risk claims and route them for preemptive correction. When denials occur, dedicated teams appeal with documentation and code corrections.
Reporting & analytics
Real-time dashboards show A/R days, net collection rates, denial trends, and payer performance. These metrics let leaders evaluate ROI and vendor performance quickly.
Key benefits offered by Healthcare RCM Companies in USA
Working with specialized RCM vendors provides measurable benefits:
Faster cash flow
Vendors accelerate claim cycles with clean claim submission and rapid follow-up. Faster reimbursement reduces reliance on reserves and improves operational stability.
Lower denials and rework
Pre-submission edits, payer-specific rules, and denial prediction algorithms reduce the denial rate. Fewer denials mean less staff time spent on appeals and more predictable revenue.
Better coding and compliance
Skilled coders plus AI tools improve ICD and IPDRG coding accuracy. This reduces audits and maximizes legitimate reimbursement. Healthcare RCM Companies in USA often include continuous coding audits and training.
Higher collections and revenue uplift
Improved coding, fewer denials, and effective follow-up increase net collections. Many clinics see double-digit gains in collection rates within months.
HIPAA compliance and security
Reputable vendors run HIPAA-compliant processes, encrypted data flows, and routine security audits. This protects patient data and reduces regulatory risk.
Technology differentiators to evaluate
Not all vendors are equal. Look for these technology features when vetting Healthcare RCM Companies in USA:
AI-powered coding
Automated ICD coding engines with machine learning accelerate coding and reduce human error. Pairing AI with certified coders yields the best accuracy.
Denial prediction and prevention
Predictive models flag high-risk claims before submission. This proactive approach reduces denials and increases first-pass acceptance.
Secure cloud and real-time dashboards
Secure cloud platforms let practices view revenue metrics in real time and collaborate with vendor teams. Transparency improves decision-making.
Integration and interoperability
Vendors should integrate with EHRs and clearinghouses to avoid manual reentry and maintain data integrity.
How Healthcare RCM Companies in USA structure their services
Full RCM outsourcing
Vendors take over the entire revenue cycle, from scheduling to final appeals. This model suits clinics that want operational relief.
Hybrid models
Some practices retain front-office tasks and outsource coding, billing, and appeals. Hybrid approaches balance control and cost savings.
Specialized services
Vendors may offer targeted offerings such as Physician Digital Marketing Services , AI-Powered IPDRG Coding Solutions , or Healthcare Staff Recruitment Assistance.
Typical vendor process: onboarding to reporting
Understand the typical steps before signing a contract with Healthcare RCM Companies in USA.
Onboarding
Vendors map workflows, connect to EHRs, train staff, and set KPIs. Good onboarding reduces disruption and accelerates benefits.
Claims submission
After mapping rules, the vendor scrubs claims, submits them, and sets automated follow-up schedules.
Coding workflows
Automated ICD Coding Tool with AI suggests codes; certified coders review and finalize them for submission.
Payment posting
Payments land in the clearinghouse; the vendor posts them and reconciles short pays or underpayments.
Denial management
Denials trigger root-cause analysis, corrective workflow changes, and appeals. Denial Prediction and Prevention Services cut repeat denials.
Reporting and reviews
Vendors provide dashboards with KPI trends and monthly reviews to keep leadership informed.
Pricing models and what to watch for
Pricing varies. Common models include percentage of collections, per-claim fees, or fixed monthly fees. Ask about:
• Fees for clean vs. complex claims.
• Contract length and exit clauses.
• Fee transparency for denials, appeals, and audits.
Selecting an RCM partner: evaluation checklist
Use a checklist to compare Healthcare RCM Companies in USA:
Performance and outcomes
Request historical metrics: first-pass acceptance, denial rate, net collection rate, and average days in A/R.
Technology and integration
Confirm EHR compatibility, API access, and real-time reporting.
Compliance and security
Ask for HIPAA audit reports, SOC 2 status, and data encryption details.
Staffing and expertise
Verify coder certification, payer specialists, and continuous training programs.
Client support
Confirm SLAs for response times, escalation paths, and regular business reviews.
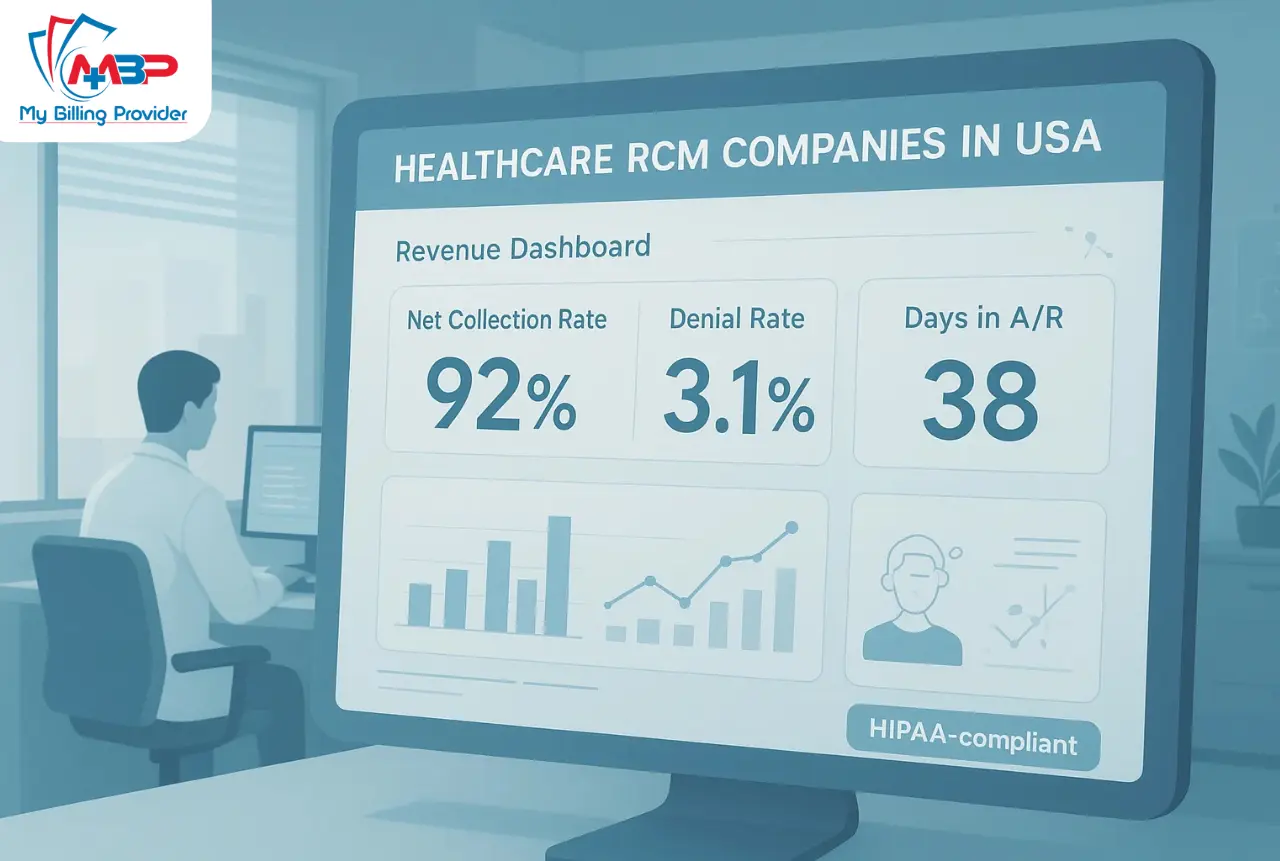
Short case example with numbers
example: Clinic X is a 6-provider primary care group that moved billing to a specialized vendor among Healthcare RCM Companies in USA. Baseline metrics: monthly billed charges $750,000; net collection rate 88%; A/R days 62. After six months:
• Clean claim rate rose from 82% to 93%.
• Denial rate dropped from 7.2% to 3.1%.
• Net collection rate increased from 88% to 106% of previous baseline, driven by faster follow-ups and corrections.
• A/R days reduced from 62 to 38.
Net result: Clinic X saw an 18% net collection increase in 6 months and recovered $92,000 in previously underpaid claims.
Risk management, audits, and trust factors
Trust matters. Verify that Healthcare RCM Companies in USA provide:
• Continuous coding audits and quality checks.
• HIPAA-compliant policies and breach protocols.
• Transparent reporting and client access.
• References and case studies.
Include about text:
At My Billing Provider, we combine cutting-edge technology with personalized service to maximize reimbursement and minimize disruption.
How to measure success with an RCM partner
Track these core KPIs:
• Net collection rate.
• Days in A/R.
• Denial rate and reasons.
• First-pass acceptance rate.
• Time to payment.
Regular vendor scorecards show whether an RCM partner meets expectations.
Common objections and quick responses
“We’ll lose control of billing.”
A structured SLA, regular reporting, and hybrid models let practices retain control while outsourcing time-consuming tasks.
“Will outsourcing cost more?”
Savings from fewer denials, lower staffing costs, and higher collections often offset vendor fees.
“How secure is my data?”
Top firms use encrypted cloud environments, regular audits, and strict access controls to meet HIPAA rules.
Services to look for in top Healthcare RCM Companies in USA
Look for vendors offering a comprehensive service suite:
• Revenue Cycle Management Solutions
• AI-Powered IPDRG Coding Solutions
• Physician Digital Marketing Services
• Insurance Payment Verification Services
• Automated ICD Coding Tool with AI
• Denial Prediction and Prevention Services
• Healthcare Staff Recruitment Assistance
Questions to ask during vendor demos
• How do you handle payer-specific edits?
• What is your average denial rate for similar practices?
• Can I see sample dashboards?
• How do you measure coder accuracy?
• What SLAs do you commit to for AR follow-up?
Regulatory and coding compliance notes
Maintain attention on ICD updates and DRG/IPDRG coding guidelines. Vendors should provide regular coder training and compliance reviews. For regulatory background, consult authoritative sources such as for coding standards and for HIPAA guidance.
Final checklist before signing a contract
• Confirm KPIs and reporting cadence.
• Review fee structure and hidden costs.
• Ask for client references and outcomes.
• Ensure termination terms are fair.
• Plan transition and staff training.
Conclusion — selecting the right partner
Healthcare RCM Companies in USA play a pivotal role in clinic financial health. The right partner combines secure technology, certified staff, proven processes, and clear outcomes. When choosing a vendor, emphasize measurable results, tech integration, coding accuracy (ICD and IPDRG), and HIPAA compliance. The right RCM partner turns billing from a cost center into a predictable revenue engine.
Call to action:
Request a free RCM audit to benchmark your current revenue performance.
Schedule an AI coding demo to see Automated ICD Coding Tool with AI and AI-Powered IPDRG Coding Solutions in action.
FAQs
- What services do Healthcare RCM Companies in USA provide?
Most offer patient access, coding, claims submission, payment posting, denial management, reporting, and compliance services. Specialized offerings include AI-powered coding, denial prediction, and staff recruitment. - How quickly can a clinic see results after switching RCM vendors?
Many clinics see measurable improvement in 3–6 months, including reduced A/R days and lower denial rates, depending on onboarding speed and claim volumes. - Are AI coding tools reliable for complex cases?
AI speeds coding and flags suggestions, but the best approach pairs AI with certified coders to review complex or ambiguous cases for maximum accuracy. - What KPIs should I track with a vendor?
Track net collection rate, days in A/R, denial rate, first-pass acceptance, and time to payment. These show financial and operational performance. - How do vendors maintain HIPAA compliance?
Top vendors use encrypted storage, role-based access, staff training, formal breach protocols, and regular security audits to meet HIPAA standards. - Do RCM vendors handle appeals and audits?
Yes. Denial management teams file appeals, submit medical records, and perform root-cause analysis. Continuous audits help prevent recurring errors. - What pricing models do Healthcare RCM Companies in USA use?
Common models include percentage of collections, per-claim fees, or flat monthly fees. Always review contract terms for hidden charges and exit clauses. - Will outsourcing RCM reduce staff jobs?
Outsourcing reallocates work. Many practices repurpose staff into patient-facing roles or higher-value revenue tasks while vendors handle specialized billing operations. - How important is EHR integration?
Very important. Good EHR integration reduces manual entry, speeds claim cycles, and improves coding accuracy. - Can small clinics benefit from RCM vendors?
Yes. Even small practices gain from improved collections, lower denials, and access to specialist knowledge and technology without hiring large billing teams.