The financial tightrope for hospitals is precarious. As we approach 2025, the era of “doing more with less” has shifted into a critical phase of operational survival. While clinical teams work tirelessly to improve patient outcomes, financial leaders are facing a perfect storm of economic pressures that threaten the viability of healthcare institutions.
Recent industry analysis indicates that despite a slight stabilization in post-pandemic volumes, hospital operating margins remain razor-thin. The difference between being in the black and falling into the red now hinges almost entirely on the efficiency of the revenue cycle. It is no longer enough to just bill for services; organizations must deploy sophisticated, proactive Revenue Cycle Management Solutions to plug leakage at every stage.
In 2025, the challenges aren’t just bigger versions of old problems; they are evolving dramatically. From payers weaponizing artificial intelligence to deny claims, to the rising tide of patient financial responsibility, the playbook for healthcare finance needs an immediate rewrite.
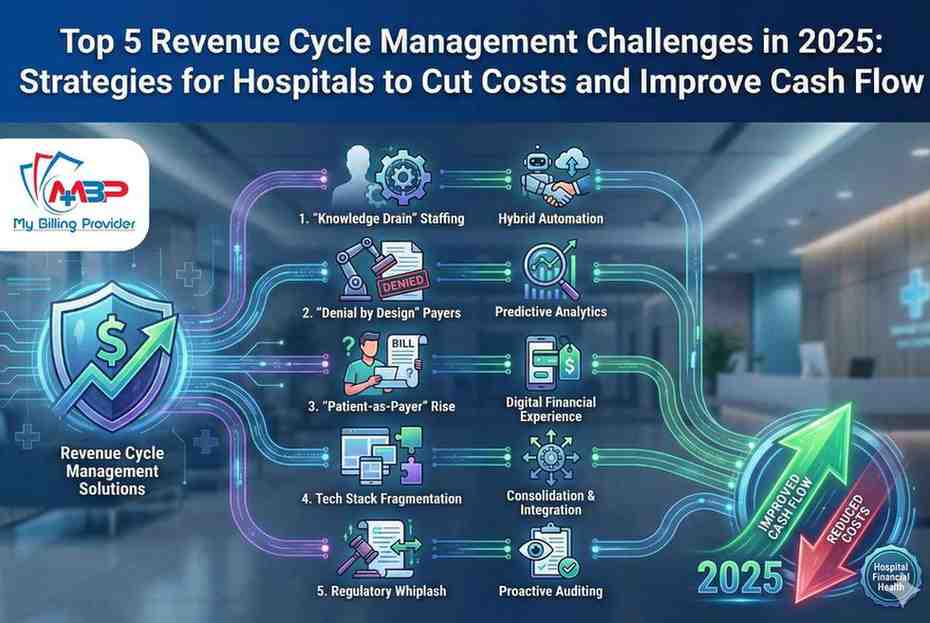
Based on deep industry research and emerging trends, here are the top five RCM challenges hospitals will face in 2025, along with strategic approaches to secure your financial health.
1. The “Knowledge Drain”: Staffing Shortages Meets Complexity
While the acute “Great Resignation” may have slowed, its long-term effects are crippling hospital RCM departments in 2025. We are witnessing a severe “knowledge drain.” The veteran coders, the billing specialists who knew payer nuances by heart, and the seasoned A/R follow-up teams have largely retired or moved to different sectors.
The 2025 Reality
They have been replaced by a newer, less experienced workforce that is facing increasingly complex billing rules. Training these new staff members is expensive and time-consuming, and the learning curve is steep. The result is an increase in preventable errors—simple coding mistakes or missed authorization requirements—that lead to immediate denials.
Strategic Path Forward: Hybrid Automation
Hospitals cannot hire their way out of this problem. The strategy for 2025 must focus on augmenting human capability with technology. This means automating repetitive, low-value tasks like claim status checks and eligibility verification to free up your limited staff for complex denial resolution. It also means considering specialized partners who can inject immediate expertise without the overhead of in-house training.
2. The “Denial by Design” Payer Landscape
If you feel like payers are denying claims faster and more frequently, you aren’t imagining it. Recent reports highlight a significant upward trend in initial denial rates across the board.
The 2025 Reality: The AI Arms Race
In 2025, payers are heavily leveraging AI and machine learning algorithms to scrutinize claims with unprecedented speed. They are identifying minute discrepancies in clinical documentation versus coding that human reviewers would miss. Furthermore, prior authorization requirements are expanding into new therapeutic areas, creating administrative bottlenecks that delay care and revenue.
Hospitals relying on manual appeals processes are bringing a knife to a gunfight. By the time a human biller reviews the denial, the clock is already ticking against timely filing limits.
Strategic Path Forward: Predictive Analytics
To combat this, hospitals must shift from reactive denial management to proactive denial prevention. This requires implementing advanced Revenue Cycle Management Solutions capable of predictive analytics. These tools analyze claims against historical payer behavior before submission, flagging potential denial risks so they can be corrected upfront. The goal is to submit a “clean claim” that is hardened against algorithmic scrutiny.
3. The Rise of the “Patient-as-Payer”
High-Deductible Health Plans (HDHPs) are now the standard. For many hospitals, the patient has become the second or third largest “payer” after Medicare and major commercial insurers. This fundamental shift requires a complete overhaul of collection strategies.
The 2025 Reality: Bad Debt and Consumer Friction
Traditional RCM was built to bill institutions, not individuals. Sending a confusing paper statement 60 days after discharge to a patient facing a $5,000 deductible is a failed strategy in 2025. It leads to soaring bad debt, uncomfortable collection calls, and plummeted patient satisfaction scores.
Strategic Path Forward: The Digital Financial Experience
Healthcare needs to adopt the retail e-commerce mindset. Strategies must include:
- True Price Transparency: Providing accurate out-of-pocket estimates before service.
- Point-of-Service Collections: Engaging patients financially when they are most engaged clinically.
- Flexible Payment Options: Offering interest-free payment plans and digital wallets through a mobile-friendly portal.
Improving cash flow here isn’t just about collections; it’s about improving the patient financial experience so they are willing and able to pay.
Visualizing the Shift: Traditional vs. 2025 RCM Strategy
| Challenge Area | Traditional Approach (Failing) | 2025 Strategic Approach |
| Staffing | Constant hiring/training cycles. | Hybrid model: Tech automation + specialized outsourcing partners. |
| Payer Denials | Reactive appeals after denial. | Proactive AI-driven denial prediction before submission. |
| Patient Collections | Post-care paper statements. | Pre-care estimates and digital, flexible payment options. |
4. Tech Stack Fragmentation and Data Silos
Over the past decade, hospitals have acquired numerous point solutions—one vendor for eligibility, another for coding queries, a third for patient portals. While intended to solve specific problems, this has created a fragmented ecosystem in 2025.
The 2025 Reality: Operational Inefficiency
These systems rarely communicate seamlessly with the core Electronic Health Record (EHR). RCM staff spend valuable time logging in and out of different portals, manually transferring data, or trying to reconcile conflicting information. This “swivel-chair interoperability” is a major source of inefficiency, data loss, and increased days in A/R.
Strategic Path Forward: Consolidation and Integration
Hospitals must rationalize their tech stacks. The focus should be on end-to-end platforms or solutions with robust APIs that integrate directly into the EHR workflow. Reducing the number of vendors simplifies management, centralizes data, and provides a “single source of truth” for the financial health of the organization.
5. Regulatory Whiplash and Compliance Fatigue
Regulatory requirements in healthcare are never static. In 2025, hospitals are still grappling with the evolving nuances of the No Surprises Act, price transparency enforcement, and changing Medicare coding guidelines.
The 2025 Reality: The Cost of Non-Compliance
The government is stepping up enforcement. Non-compliance is no longer just a risk of a slap on the wrist; it carries significant financial penalties that can wipe out margins. Furthermore, the administrative burden of constantly updating workflows to meet new regulations is exhausting already stretched RCM teams.
Strategic Path Forward: Proactive Auditing
Waiting for an external audit is a dangerous strategy. Hospitals need continuous, internal auditing processes that mirror regulatory scrutiny. This involves regularly reviewing coding accuracy, ensuring Good Faith Estimates are compliant, and verifying that public-facing pricing files are current.
The “My Billing Provider” Advantage: Navigating 2025 Together
The challenges outlined above prove that generic, out-of-the-box RCM strategies are insufficient for the financial realities of 2025. Hospitals need partners who provide more than just software; they need bespoke strategies and deep expertise.
This is where My Billing Provider steps in to bridge the gap between operational strain and financial stability.
We understand that a rural community hospital has different RCM stress points than a large urban academic center. We don’t offer cookie-cutter approaches. Our methodology begins with a forensic-level analysis of your current revenue cycle to identify the specific “leaks”—whether they stem from front-end registration errors, mid-cycle coding gaps, or back-end denial mismanagement.
By partnering with My Billing Provider, you address the 2025 challenges head-on:
- Combating Staff Shortages: Our skilled team acts as an extension of your business, providing immediate expertise in complex claims processing and compliance without the training overhead.
- Outsmarting Payer Algorithms: We leverage innovative technology to scrub claims and predict denials before they happen, ensuring faster reimbursement.
- Enhancing Patient Payments: We help streamline the patient financial journey, making it easier for patients to understand their obligations and pay promptly.
Conclusion: Time to Act
In 2025, revenue cycle excellence is not a back-office function; it is a strategic imperative for hospital survival. The costs of inaction—increasing denials, ballooning bad debt, and regulatory penalties—are too high.
Don’t let the financial challenges of 2025 dictate your hospital’s future. Take control of your cash flow and refocus your energy on what matters most: high-quality patient care.
Contact My Billing Provider today to set up a consultation and learn more about how our specialized solutions can improve the financial health of your practice.